Policies to improve the Availability, Affordability and Access (the three ‘A’s) of Vaccines
April 22, 2025
Executive summary
Currently, vaccines can protect people against over twenty diseases and there is a rich pipeline of new vaccines in development.i However, there are significant differences in market access pathways across Member States and concerning issues in roles and decision-making criteria. The composition of National Immunisation Technical Advisory Groups (NITAG), critical in implementing National Immunisation Programmes (NIP), varies widely among countries. Only 16 out of 22 European NITAGs include the required specialists in vaccinology and immunology.ii Despite the well-established, cost-effective role of immunisation in disease prevention, a staggering 77% of European countries spend less than 0.5% of their healthcare budget on immunisation, with only a few increasing their budgets to adequately address their public health needs.iii These constraints, among other issues, lead to delays, with some countries taking more than 6 years for vaccines to become accessible.iv Consequently, there are discrepancies across Europe in terms of reaching target populations and achieving the recommended vaccination coverage rates.
Charles River Associates (‘CRA’) was commissioned by Vaccines Europe (‘VE’) to develop an analysis of the policy issues affecting the availability, affordability, and access (AAA) of vaccines in Europe. The aim was to define the three ‘A’s affecting routine vaccines, collect evidence on the cause of each of the three ’A’s for the inclusion of these vaccines in NIPs, and how policy solutions could address these issues across the vaccine market access (VMA) pathway. In this context, routine vaccines refer to vaccines that are used as part of an ongoing, systemic vaccination programme including vaccines across the life-course. These findings have been tested and validated with various vaccine experts, including NITAG members, national payers, physicians, academics, and technical officers for the WHO.
Defining availability, affordability, and access for vaccines
The three ‘A’s—availability, affordability, and access for vaccines—have received more attention following the COVID-19 pandemic. A conceptual framework was developed with VE members including a definition of each of the A’s, an associated goal, and showing the interdependency of the three A’s by presenting them as a cascade, rather than a strictly linear pathway. This is a simplification, as, in reality, decisions in European countries can occur in parallel, overlapping across areas. For example, budgetary discussions may happen concurrently with NIP considerations. However, if the goal for the three A’s were reached this would support optimal vaccine uptake across Europe.

Underlying causes of differences in availability
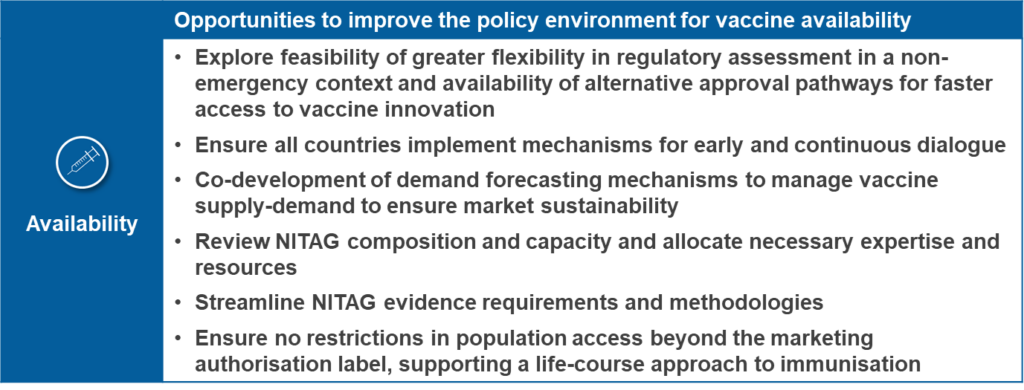
Vaccine availability is dependent on securing market authorisation by the relevant regulator (the European Medicines Agency (EMA) in Europe) after which manufacturers must then undergo individual national assessment for the vaccine’s inclusion in the NIP. Key steps at the national level may include horizon scanning, early advice, NITAG assessment, and recommendations for consideration of vaccines into NIP. The underlying causes of differences in availability include:
- Delays to marketing authorisation and the timeliness of regulatory revisions
- Lack of early and continuous dialogue from recommending bodies with industry to better anticipate NITAG review timelines, HTA review procedures and demand planning for new and existing vaccines
- Misalignment of evidence requirements and evidence value due to varying healthcare system processes
- Heterogenous national assessment systems with limited life-course vaccine prioritisation and lack of transparency with vaccine manufacturers and the public
- Restrictions in the recommended target population due to the influence of budgetary concerns rather than public health considerations
Underlying causes of differences in affordability
The funding provisions for immunisation programmes need to adapt to reflect the introduction of new vaccines. The underlying differences related to affordability are driven by the availability of budget to facilitate the implementation of vaccine recommendations including:
- Insufficient budget allocated for effective implementation of NIPs to fulfil the needs of target populations
- Inability of budgets to have the flexibility to adapt to the changing public health needs and ongoing vaccine innovation
- Lack of alignment between national and regional decision-makers on public health priorities and budget allocation
Underlying causes of differences in access
The underlying differences in access relate to the effectiveness of implementing national immunisation programmes and supporting enablers that result in optimal uptake of vaccines in target populations. The underlying causes of differences in access include:
- Procurement practices that reduce market attractiveness and limit supply adaptability to evolution of population needs that do not account for overall vaccine manufacturing challenges
- Limited expansion of vaccination access points for effective implementation of life-course immunisation to support equitable access
- Differences in guidelines and involvement of HCPs in vaccine administration
- Policies affecting equity and individual patient affordability, e.g., co-payments
- Lack of infrastructure to collect, monitor and evaluate RWE to support appropriate vaccine uptake in target populations, limiting VCR
- Lack of comprehensive education for HCPs and the public, increasing vaccine hesitancy and hindering acceptance of new vaccines
Policy opportunities
Given the multifactorial root causes, the need for a dialogue on how to improve the three ‘A’s for vaccines is clear. Drawing on the key findings and supporting evidence of factors affecting the three A’s, we identified a number of opportunities to improve the policy environment to address the underlying causes of differences across the three ‘A’s. Given the multifactorial root causes, there is a need for a multi-stakeholder dialogue on how to improve the policy environment. Only by addressing the underlying causes of variation in availability, affordability and access will European patients, healthcare systems, and broader society yield the benefits that vaccines can deliver.